Q+A with Valerie Hoffman, PhD., the Head of Research at Meru Health
Reference: Kroenke, K., West, S.L., Swindle, R., Gilsenan, A., Eckert, G.J., Dolor, R., Stang, P., Zhou, X.H.,
Hays, R. and Weinberger, M., 2001. Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: a randomized trial. Jama, 286(23), pp.2947-2955.
How to measure the quality and efficacy of mental health treatments, whether it’s psychotherapy, antidepressants, or other types of care, has been a question mark in the mental health industry for decades. Unlike in physiological analysis where we can determine the improvements or worsening of someone’s state by objective markers (e.g. blood tests), in mental healthcare, changes in symptoms are often based on subjective feelings of the patient either self-reported via unstandardized assessments or as interpreted by their mental health provider. An important first step in building effective new mental health solutions is to define how to appropriately measure treatment efficacy. Valerie Hoffman, Head of Research at Meru Health, has been studying psychiatric epidemiology for two decades and published over 80 peer-reviewed research papers and now explains to us how to measure the efficacy of depression and anxiety treatments and why it is so important to do so.
Q
Why is it imperative that we use standardized scales in mental health treatment?
A
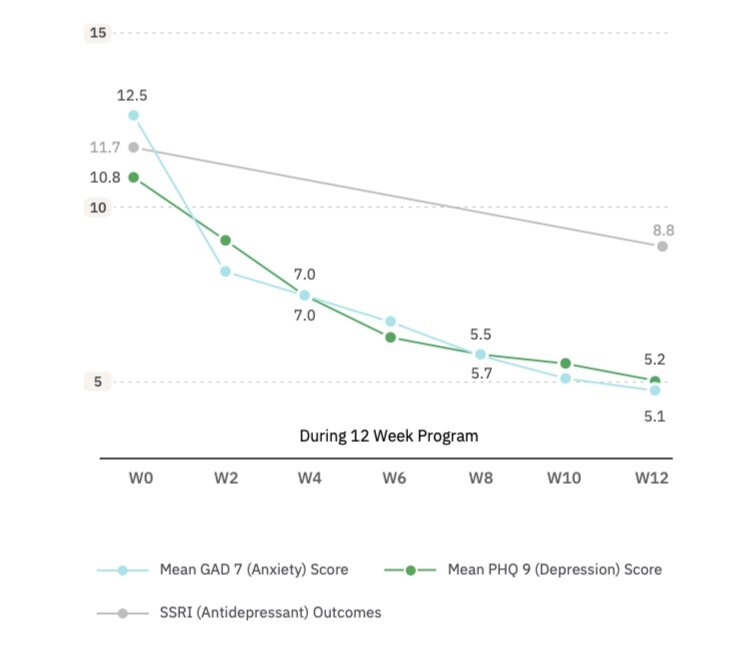
Using standardized scales like the GAD-7 for anxiety or the PHQ-9 for depression gives us the best chance of measuring whether treatment is working for a particular patient. Standardized tools have both demonstrated validity (accurately measuring what they intend to measure) as well as reliability (ability to consistently find the same thing if repeated). Standardized measures also are sensitive enough to determine even small changes over time and typically have established norms to be able to use as benchmarks. We all know that mental healthcare is not one size fits all and we should do our best to provide everyone a treatment program that is right for their needs and adjust it if we see that the treatment is not working and that the patient’s condition is deteriorating. Giving patients an opportunity to complete standardized assessments over the course of treatment also allows us a way to ensure that the quality of the care given is high. Imagine a therapist is seeing a client who is not improving on a standardized assessment – that provider could then revisit the quality of the care provided to make sure it was the best possible. Finally, using a standardized instrument routinely during the course of treatment and sharing the results with the patient can provide the needed reinforcement to validate the hard work that the patient is doing to help him- or herself recover. These standardized assessments can be done in very little time and, from my perspective, provide so much benefit to both patients and providers during the course of treatment that their use should be a “no brainer”!
Q
Are there some objective markers to determine the treatment efficacy?
A
Excitingly, yes! Besides the self-reported PHQ-9 scale for Depression and the GAD-7 scale for anxiety, changes in the body’s physiology can be measured by using a Heart Rate Variability (HRV) device. The device is clipped to the earlobe and it measures the beat-to-beat changes in that patient’s heart rate while they engage in a practice of guided, slow-paced breathing called HRV-biofeedback (or HRVB for short). The device provides a measure of each patient’s physiological response to stress, which is a common factor behind many mental disorders. The device feedback teaches patients how to use their breath to improve their stress response and provides both the patient and provider with an objective measure of success with this practice. It can also track how changes in these physiological processes correlate with changes in the self-reported PHQ-9 depression and GAD-7 anxiety outcomes.
Q
How often should measures/assessments be taken?
A
Here at Meru Health, we ask patients to complete the PHQ-9 and GAD-7 measures before the 12-week program starts, every two weeks during the program, and even after the program at regular intervals to be able to examine long-term outcomes of the program participation. It is so important to continue these measurements even after the program ends to enable us to study the program’s impact on relapse and long-term recovery. We know from extensive research that 50% of people end up relapsing after their first depressive episode and this statistic increases to 80% when looking at those experiencing their second or greater episode. Our goal at Meru Health is to provide long-term tools and strategies during the program to empower them to get better and stay better long-term. Not only does it save provider resources and money, but ultimately reduces the burden of suffering from depression and anxiety long term, so that people can live their best lives possible.
Q
Can you shed light on how these measures help you improve mental health treatment in practice?
A
At Meru Health, we are conducting clinical trials with universities such as Stanford and Harvard as a way to continuously improve our treatment program. We recently looked at patients who completed our program after we added the HRV-B component to those who completed our program before adding the HRV-B component and found some really interesting insights. After matching the two groups for gender, age, and beginning severity of depression, we found that those who participated in our program after adding HRV-B were over twice as likely to experience significant symptom improvements. Searching for clues about the program’s most efficacious components is no easy task, however, as there is no “one size fits all” treatment that works for everyone. As we move forward, it will be increasingly necessary to study this variability in treatment response – it’s a start to solving this very complex puzzle of how to most successfully treat depression for each individual patient.
Valerie Hoffman holds a Ph.D. in Psychiatric Epidemiology from Johns Hopkins Bloomberg School of Public Health, and a Master’s degree in Public Health from Yale University. She has been studying psychiatric epidemiology for two decades and published over 70 peer-reviewed research papers. Valerie is the Head of Research at Meru Health, where she is part of developing a novel, technology-based integrated mental health solution to battle depression, anxiety, and burnout.





